Background: Sarcopenia is characterized by the loss of muscle mass and strength, commonly observed in older adults. Sarcopenia has become a significant prognostic factor in various cancer types, including diffuse large B-cell lymphoma (DLBCL). Vitamin D, an essential nutrient for bone health and immune function, has been studied as a potential factor in preventing and treating sarcopenia. Vitamin D deficiency has also been reported to be a poor prognostic factor for DLBCL. Therefore, we investigated the relationship between skeletal muscle index (SMI) and vitamin D and its prognostic impact on DLBCL.
Methods: We retrospectively analyzed 213 newly diagnosed DLBCL patients from 2012 to 2022 at Gifu University Hospital. The standard regimens in this study included R-CHOP or R-THP-COP. The muscle mass of the third lumbar vertebra was measured and converted to the SMI by dividing the muscle mass by the square of the height (cm 2/m 2). The sex-specific cutoffs for SMI (42 cm 2/m 2 in males and 38 cm 2/m 2 in females) were used to stratify into low and high SMI groups according to The Japan Society of Hepatology guideline. Serum 25-hydroxyvitamin D [25(OH)D] was measured by the electrochemiluminescence method using serum cryopreserved during diagnosis. For analysis, 25(OH)D values were categorized according to three conditions: deficient (< 20 ng/mL), insufficient (20-29 ng/mL), and normal (≥ 30 ng/mL).
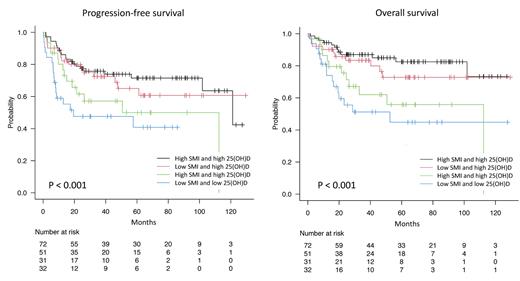
Results: After excluding ineligible patients, 186 patients were included. The median age was 71 (20-93) years, with 80% of the patients over 60. The median SMI was 39.8 cm 2/m 2 in males (7.4-76.0 cm 2/m 2) and 33.7 cm 2/m 2 (6.9-63.0 cm 2/m 2) in females, with 38 (36%) males and 45 (56%) females determined to have low SMI. The median 25(OH)D was 13.0 ng/mL (4.0-27.1 ng/mL); 35 (19%) patients were vitamin D deficient, 151 (81%) were vitamin D insufficient, and no patient had normal vitamin D. There was no significant difference in 25(OH)D between the low SMI and high SMI groups (P = 0.189). However, when analyzed separately by gender, 25(OH)D was significantly lower in males with the low SMI groups (P = 0.017) but not in females (P = 0.359). Using the ROC curve, the optimal 25(OH)D cutoff for progression-free survival (PFS) and overall survival (OS) was 9.6 ng/mL. Multivariable analysis using the COX proportional hazards model with gender, cell of origin of DLBCL, International Prognostic Index, low SMI, and low 25(OH)D as covariates showed that the hazard ratio (HR) of low SMI for PFS was 1.42 [95% confidential interval (CI) 0.86-2.37, P = 0.17] and OS was 1.38 (95% CI 0.77-2.47, P = 0.28), and the HR of low 25(OH)D for PFS was 2.45 (95% CI 1.47-4.07, P < 0.001) and OS was 3.19 (95% CI 1.76-5.77). P < 0.001). When SMI and 25(OH)D were combined, both PFS and OS could be stratified into four groups, with patients with low SMI and low 25(OH)D having the poorest prognosis (5-year PFS: 40.8%, 5-year OS: 44.3%). Those with high SMI and high 25(OH)D had the best prognosis (5-year PFS: 71.5%, 5-year OS: 82.5%).
Conclusion: This study is the first study investigating the relationship between SMI, vitamin D, and survival outcomes in patients with DLBCL. Our study suggests that vitamin D deficiency and low SMI may synergistically affect the prognosis of DLBCL patients. These findings highlight the importance of assessing nutritional status and muscle health in DLBCL patients. Future prospective studies are needed to confirm our findings and to investigate the potential benefits of vitamin D supplementation and interventions to prevent or treat sarcopenia in DLBCL patients.
Disclosures
Nakamura:Sumitomo Pharma: Honoraria; Kyowa Kirin: Honoraria; AbbVie: Honoraria; MSD: Honoraria; Chugai Pharmaceutical: Honoraria; Sanofi: Honoraria; Janssen Pharmaceutical: Honoraria; Eisai: Honoraria; Novartis Pharmaceuticals: Honoraria; Nippon Kayaku: Honoraria.